Unsupportive environments and limited policies: Pregnancy, postpartum, and birth during incarceration
Making up for a serious gap in government data collection and understanding, researchers are discovering what pregnant incarcerated women should expect when they’re expecting (or when they give birth while in custody). Findings indicate that jails, prisons, and youth facilities have yet to adequately recognize pregnancy and postpartum needs either in policy or in practice.
by Leah Wang, August 19, 2021
Recently published findings from the groundbreaking Pregnancy in Prison Statistics (PIPS) Project and other datasets shed light on a common but rarely discussed experience: being pregnant, postpartum or giving birth while incarcerated. Spearheaded by Dr. Carolyn Sufrin of the Johns Hopkins University School of Medicine and School of Public Health, this series of studies is our best look yet at pregnancy prevalence and outcomes in U.S. jails, prisons, and youth facilities.
In total, 22 state prison systems, all federal prisons, 6 jails, and 3 youth confinement systems participated in the PIPS Project, a systematic study of pregnancy and its outcomes among incarcerated women. Historically, the government has not collected data about carceral pregnancy on a regular basis, meaning no national effort has been made to understand maternity care for thousands of incarcerated pregnant women.1 The project’s sample represents 57% of all women in prison, 5% of all women in jail and about 3% of young women in youth facilities.
Our takeaway: Carceral pregnancy, whether in jail, prison, or youth confinement, is characterized by a lack of supportive policies and practices. Some of the major findings to come out of these publications are:
- There are an estimated 58,000 admissions of pregnant women into jails and prisons every year, and thousands give birth or have other outcomes while still incarcerated. Pregnancy rates among confined youth were similar to those among adults.
- In some state prison systems, miscarriage, premature birth, and cesarean section rates were higher than national rates among the general population.
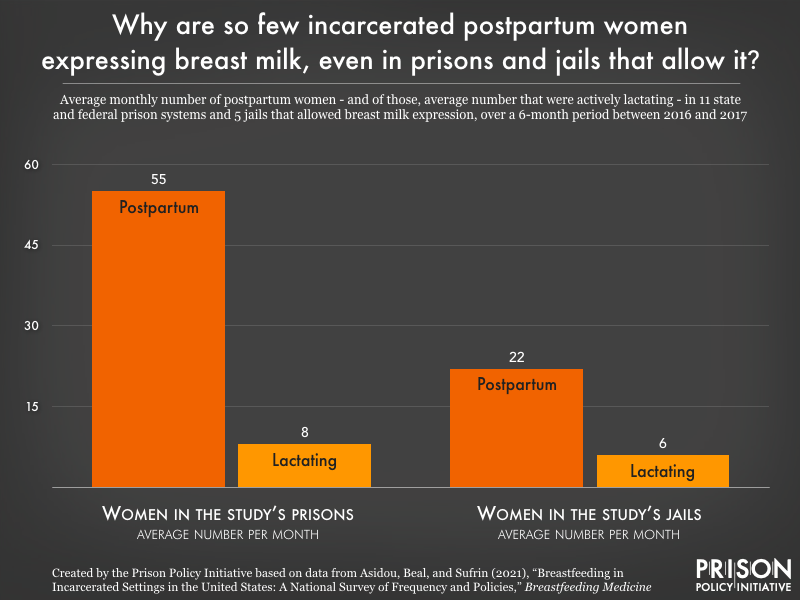
- Only one-third of prisons and jails had any written policy about breastfeeding or lactation, and even where policies supporting lactation did exist, relatively few women were actually breastfeeding or pumping.
- There are an estimated 8,000 admissions of pregnant women with opioid use disorder (OUD) into prisons and jails each year, but long-term treatment using medication is the exception, not the rule.
- A related (non-PIPS Project) study finds paternal incarceration is also linked to adverse birth outcomes like low birth weight, which are widely known to impact long-term health.
The researchers’ findings add complexity to a growing body of literature and consensus linking incarceration to negative health impacts. And although PIPS Project data can’t be broken down by race, ethnicity, or gender identity, measuring the scale and outcomes of pregnancies in prison and jail is a major public health research accomplishment. The fact that academic researchers had to conduct this research to fill the data gap – and the shortage of appropriate policies they found – makes it clear that many correctional agencies have yet to even acknowledge the needs of pregnant incarcerated women.
Every year, thousands of incarcerated expecting mothers and babies face adverse outcomes from exposure to incarceration
Over the 12 months of the Pregnancy in Prison Statistics (PIPS) study period, there were nearly 1,400 admissions of pregnant women to participating state and federal prisons with over 800 pregnancies ending in custody (births, miscarriages, and others), and over 1,600 admissions of pregnant women to jails with 224 pregnancies ending in custody. Unsurprisingly, given the short length of most jail stays, more pregnant women are admitted to jails each year, but more births take place in prisons, where the average stay is longer. Based on their data, the authors estimate that nationally, 4% of women entering prison (in line with Bureau of Justice Statistics 2016 estimates) and 3% of women admitted to jail (lower than BJS’ most recent 2002 estimates) are pregnant.
Pregnancy outcomes in prisons and jails in some places were worse than national trends across the general population. When pregnancy did end in custody, in some states like Arizona, Kansas and Minnesota, rates of miscarriage ranged from 19 to 22%, exceeding estimates of the national rate.2 In Ohio and Massachusetts, premature births exceeded the general population rate of about 10%. Among live births, which were 92% of birth outcomes in custody, one-third (32%) of these were caesarean section births, in line with the national average rate. In some states, the C-section rate was much higher, suggesting that C-sections may be taking place when not medically necessary, risking short- and long-term health problems in babies.
Pregnancy among confined youth is not uncommon, and better testing might reveal it’s even more widespread
Upon hearing about the Pregnancy in Prison Statistics (PIPS) Project, three juvenile justice systems (one state-level, and one county-level system) volunteered to complete a survey about pregnant adolescents in the custody of 17 of their “juvenile residential placement” facilities, providing a window into this population for the first time. One takeaway from the survey’s findings was that adolescent pregnancies – both in confinement, and upon release – may risk poorer outcomes because of a lack of continuity of medical care between confinement facilities and the community. Even though all three state systems provided basic prenatal care, with the typical length of stay for young women lasting a few months or less, justice-involved youth would benefit enormously from consistency in medical care throughout pregnancy.
The survey also showed that the rate of pregnancy among confined youth (3.3%) was similar to that of the adult incarcerated population (3.5%). However, the youth facilities reported less routine pregnancy testing, bolstering a 2004 study revealing that only 15-17% of 1,255 juvenile facilities nationwide tested youth for pregnancy at admission (with about two-thirds of facilities providing tests only if requested). Therefore, it’s possible the youth carceral pregnancy rate is a very conservative estimate, and that thousands of pregnant youth are going without prenatal care when their health needs are likely complicated.
Eight pregnancies ended among youth confined in the surveyed facilities during the 12-month study period, including four miscarriages, three induced abortions, and one live full-term birth. It would be misleading to view these outcomes as representative of all pregnant confined youth, but the authors
advise youth confinement facilities to be prepared for high rates of miscarriage and other adverse birth outcomes, seeing as justice-involved pregnant youth are going through highly stressful life experiences.
Services and policies regarding prenatal and postpatrum care were variable: All three juvenile systems allowed abortion, and some covered the cost; all three systems also allowed lactation through either breastfeeding or pumping. Still, the small sample size (which represented just 2.8% of all confined female youth) and the potential influence of self-selecting facilities make it difficult to draw conclusions about the experience of pregnant youth in confinement.
Breastfeeding and lactation are not guaranteed to new mothers and babies, ignoring the enormous benefits of breast milk
When the cohort of 22 prison systems and 6 jail systems described their lactation-related policies to the researchers, they painted a discouraging picture of how correctional facilities largely don’t support breastfeeding, a practice chosen by some mothers for its unique benefits.
To begin, only one-third of prisons and jails had any written policy on lactation, leaving many incarcerated women to the whims of facility staff who may not be trained in this area or understand its importance. Even where women were formally allowed to lactate, milk was sometimes discarded at the study sites due to mother-infant separation, providing only a benefit to the mother of maintaining milk supply.
Because it is a matter of health equity to provide the opportunity to lactate and breastfeed (among other parental choices), researchers extend the “further research is needed” statement in order to understand the probable racial disparities within carceral pregnancy: “…research in collaboration with current and formerly incarcerated women, specifically Black, Indigenous, and women of color, is needed to fully understand breadth of experiences and perspectives related to breastfeeding and lactation while in custody.”
Opioid use disorder among incarcerated women is treated under some circumstances, but leaves mothers without help postpartum
In addition to known medical needs during pregnancy, some women enter incarceration with other health problems. Researchers accessed six months of activity and policy related to opioid use disorder (OUD) treatment of pregnant women in the Pregnancy in Prison Statistics (PIPS) study sites and found that 26% of those entering prison and 14% entering jail had OUD.3 The gold standard of care for these women would be medication for opioid use disorder (MOUD), which is linked to better pregnancy outcomes and increased engagement with addiction treatment and other medical care.4
Twenty-two of 28 sites did offer this avenue for treatment of pregnant women in some way, but the narrow window in which they could be treated for OUD leaves much room for improvement. In most facilities offering MOUD, it would not be initiated in the facility; they would only continue someone on MOUD if they were already on it. This unfairly excludes women who were unable to begin treatment before admission; for example, if someone was in jail before being transferred to prison, their access would then depend on the jail’s policy. Postpartum, most facilities providing MOUD would discontinue treatment, showing a clear disregard for the mother’s well-being after birth.
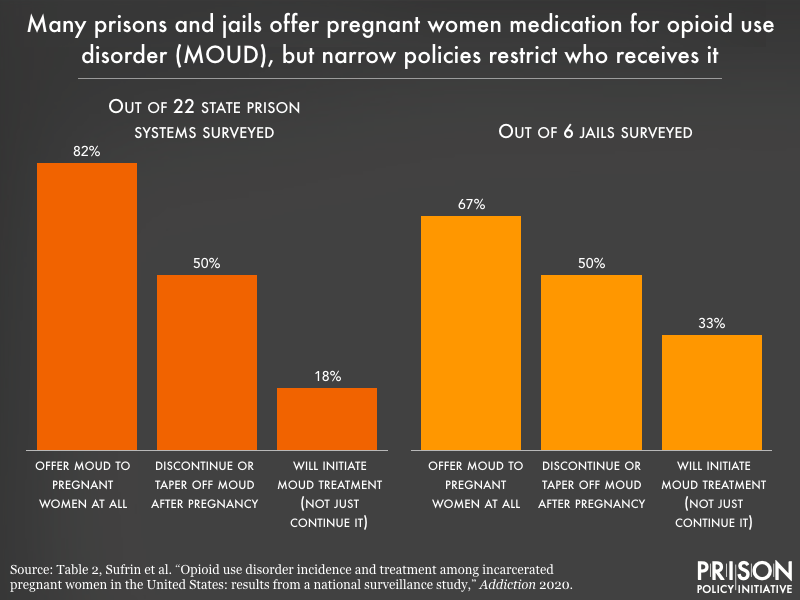
Still, one-third of surveyed sites managed OUD among pregnant women through detoxification, some with and some without medication to manage symptoms. Detox, or “medically supervised withdrawal,” can be a painful process and has a high rate of failure for pregnant women, increasing the risk of future overdose.
These exclusionary policies and practices are troubling given the fact that opioid overdose is a major cause of death for pregnant and postpartum women in the United States, and remains a huge concern for formerly incarcerated people. In Rhode Island, where MOUD has been implemented comprehensively in their unified prison-jail system, there has been a huge reduction in post-release overdose deaths; replicating their initiative would have a great impact on carceral pregnancy and postpartum outcomes.
The incarceration of fathers is also linked to worse birth outcomes
As if it’s not bad enough that incarceration prevents expecting mothers from receiving care and providing care to their babies, another recent study finds that incarcerating fathers during pregnancy or at the time of birth is also harmful to babies’ health.
In another recent study – unrelated to the Pregnancy in Prison Statistics (PIPS) project – Youngmin Yi and fellow researchers matched hundreds of thousands of birth records to jail records in New York City between 2010 and 2016, observing trends in birth weight, preterm (premature) birth, admission to the NICU (neonatal intensive care unit), and more. Paternal incarceration was associated with nearly all adverse outcomes,5 even after other characteristics of mother and father were accounted for statistically. “Exposed” to their fathers’ incarceration – even for as little as one day – babies were born with these vulnerabilities, such as low birth weight, known to have an impact later in life.
Incarcerated pregnant people and their babies deserve better care that is codified in policy
The findings by Sufrin, Asiodu, Kim and fellow researchers offer a desperately-needed look into pregnancy during incarceration. And the findings by Yi et al. contribute to an even more holistic picture of what it means to be a growing family entangled in the criminal legal system. Families experiencing pregnancy are impacted by incarceration whether the mother or the father is incarcerated, and whether or not the baby is born during the mother’s incarceration.
Both adolescents and adults in confinement should be afforded comprehensive prenatal care, including education, lactation support, and opioid use disorder treatment that continues beyond the end of pregnancy. And babies born right after or during their parents’ incarceration, who risk health issues like lower life expectancy and social and emotional challenges, deserve the chance to begin life with one or both parents as much as possible. These efforts and programs should be clearly written into agency policy so that facility staff can be trained and expected to provide care.
One way that prisons and jails can begin to assess and improve their care for pregnant women is by reviewing the American College of Obstetricians and Gynecologists’ recently updated comprehensive set of guidelines for carceral reproductive health care. Facilities should also consider subscribing to the National Commission on Correctional Health Care’s standards for health services, which have clear ways of addressing many of the above topics. Prisons and jails should make their policies publicly available, and create ways to keep healthy mothers and their babies together.6
Note about the language used
Throughout these publications, the terms “pregnant women” and “mother” described those people who were pregnant in custody during the study period. While we’ve deferred to the terminology used by the authors, we acknowledge that pregnancy can overlap with multiple gender identities, and our conclusions and recommendations apply to all pregnant people.
Footnotes
-
The federal Bureau of Justice Statistics estimates that in 2016, 4% of women in state prisons and 3% of women in federal prisons were pregnant at the time of admission. (Their last estimates were from 12 years prior, in 2004.) An abysmal 50% of pregnant women in state prison, and 46% in federal prison, reported receiving some form of prenatal care. The First Step Act, signed into law in 2018, calls for pregnancy prevalence and outcome data to be collected annually, but only from federal prisons, which hold a small portion of the women’s incarcerated population. So far, live birth and miscarriage data in federal prisons in 2018 and 2019 are comparable to what Sufrin et al. found from the PIPS Project in 2017. ↩
-
Miscarriage has long been difficult to track, and estimates of its frequency range from “roughly 10 to 20%” to “as many as half,” though Dr. Sufrin contends that the U.S. miscarriage rate is around 10 percent. Rates of miscarriage and other pregnancy outcomes in custody are not exactly comparable to the general population’s rates because they only refer to outcomes that took place during incarceration. Meanwhile, those who are released while still pregnant may have their outcome impacted by incarceration, but the PIPS study does not show how any exposure to incarceration is linked to their outcomes. ↩
-
The rate of opioid use among pregnant women has increased since the early 2000s, and so has the number of women locked up in jail and prison; in fact, the war on drugs dating back to the 1980s targeted pregnant women by the very nature of their pregnancy, citing “fetal endangerment” as their crime instead of providing them with the treatment they need. ↩
-
MOUD is somewhat interchangeable with medication-assisted treatment, or MAT, though MAT generally includes counseling and regards medication as part of, not fully, the treatment. Within both practices, three medications are commonly used: methadone, buprenorphine, and naltrexone, the last of which is not recommended for use during pregnancy, and was not included in this study. We mention these because methadone was found to be much more common than buprenorphine where MOUD was offered, despite buprenorphine being easier to prescribe and integrate into prison and jail settings, and having evidence of better outcomes in babies. Researchers had some ideas as to why methadone might have been the prevailing medication, such as cost or ability to treat stronger addictions, but they were not certain of the reasons. ↩
-
The birth outcomes observed were: preterm (premature) birth, categorized as 1) late, 2) early, or 3) extremely early; low birthweight (under about 5.5 pounds); small for gestational age (among full-term births); admission to the neonatal intensive care unit; low Apgar score, which is a 10-point rating system of a newborn’s respiratory and heart health; and infant death (under 1 year old). ↩
-
Some jurisdictions are starting to find solutions for this significant time during and immediately after birth. Since 2018, Los Angeles County has run a maternal program which diverts some pregnant women from jail and allows children to remain with mothers in supportive housing or at home. And in Minnesota, the recently passed Healthy Start Act will allow sentenced mothers to remain with their newborns for up to a year after birth in community-based settings. ↩



